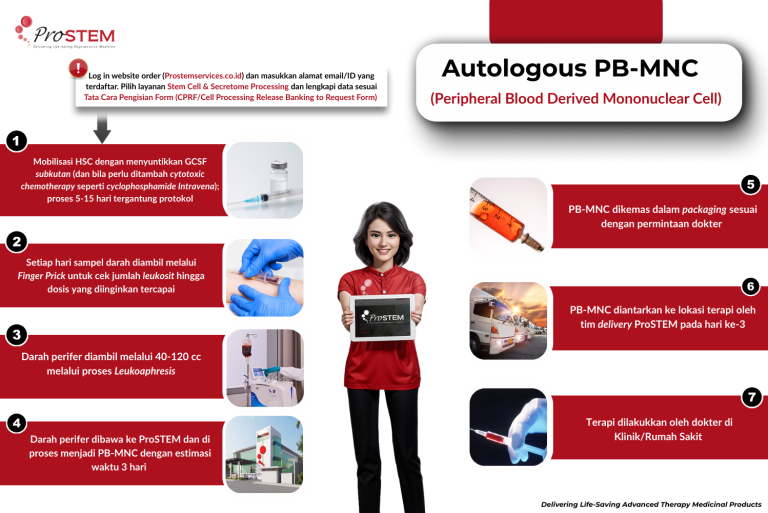
Peripheral Blood Mononuclear Cells (PB-MNC) are white blood cells derived from peripheral blood, consisting of lymphocytes (T cells, B cells, NK cells), monocytes, endothelial progenitor cells (EPC), and mesenchymal stem cells (MSC). Since peripheral blood mononuclear cells originate from bone marrow, these cells can be stimulated or mobilized by administering systemic injections of G-CSF (granulocyte colony-stimulating factor) or GM-CSF (granulocyte-macrophage colony-stimulating factor) to increase the number of PB-MNC without compromising their function and capacity1. PB-MNCs can be isolated using less invasive methods than bone marrow as a source. The following is the PB-MNC isolation procedure performed at ProSTEM. The processing workflow can be seen in the diagram below.
PB-MNC transplantation is currently used to treat patients with hematological cancers or cancers. However, further research is still needed to understand their differentiation potential and transplantation capacity.1 Just like BM-MNC, PB-MNC is also isolated using an automated separation system in ProSTEM and can be administered immediately or frozen for long-term use.
PBMNCs work through paracrine mechanisms, releasing cytokines, chemokines, growth factors, lipids, extracellular vehicles (EVs), and mRNA. The biological cascade induced by PBMNCs promotes angiogenesis and a local environment that supports adequate cell replacement and tissue integrity restoration, also through significant modulation of the regenerative activity of resident stem/progenitor cells. Autologous PBMNC cell therapy has the ability to work simultaneously on two different mechanisms of action: induction of collateral vessel formation through angiogenesis and, in addition, immunomodulatory effects through the polarization of M1 phenotype inflammatory macrophages into M2 phenotype regenerative macrophages.2
References
- Yunir E, Kurniawan F, Rezaprasga E, Wijaya IP, Suroyo I, Matondang S, Irawan C, Soewondo P. Autologous Bone-Marrow vs. Peripheral Blood Mononuclear Cells Therapy for Peripheral Artery Disease in Diabetic Patients. International Journal of Stem Cell. 2020; DOI: 10.15283/ijsc20088
- Rehak, L., Giurato, L., Monami, M., Meloni, M., Scatena, A., Panunzi, A., Manti, G. M., Caravaggi, C. M. F., & Uccioli, L. (2024). The Immune-Centric Revolution Translated into Clinical Application: Peripheral Blood Mononuclear Cell (PBMNC) Therapy in Diabetic Patients with No-Option Critical Limb-Threatening Ischemia (NO-CLTI)—Rationale and Meta-Analysis of Observational Studies. Journal of Clinical Medicine, 13(23), 7230. https://doi.org/10.3390/jcm13237230

